Why is inositol used when people are trying to get pregnant?
By Dr. Sarah Zadek ND
Inositol is a natural compound made by the human body that is involved in major pathways in metabolism, inflammation, and hormone function. It’s becoming a popular supplement for fertility due to its influence on the ovaries and key hormones like follicle stimulating hormone (FSH) and insulin, but what exactly is the benefit and how does inositol work?
What does Inositol do?
Inositol is found within our cell membranes and facilitates the sending and receiving of specific messages. Also called a “secondary messenger,” it’s like the middle man in a cascade of signals that allows certain hormones to work—specifically FSH and insulin, both of which affect the ovaries and fertility.
Inositol supports fertility in multiple ways:
- Promotes growth and development of an egg each cycle
- Helps regulate ovulation
- Promotes embryo development
In the human body, inositol exists in two forms: Myo-inositol (MI) and d-chiro inositol (DCI), with the MI form being the most abundant—typically in a 40:1 to 100:1 ratio. You’ll find higher amounts of MI in body tissues that require high amounts of energy (like the ovaries), and lower ratios (less MI and more DCI) in tissues where glucose sugar is kept in storage form, like the liver and our muscle cells. The MI form is also the most important for the ovaries because it’s the one that affects FSH1 and can impact egg quality.2
Let’s dive in a bit further on exactly how inositol helps fertility in general and why it’s used so often in polycystic ovary syndrome (PCOS).
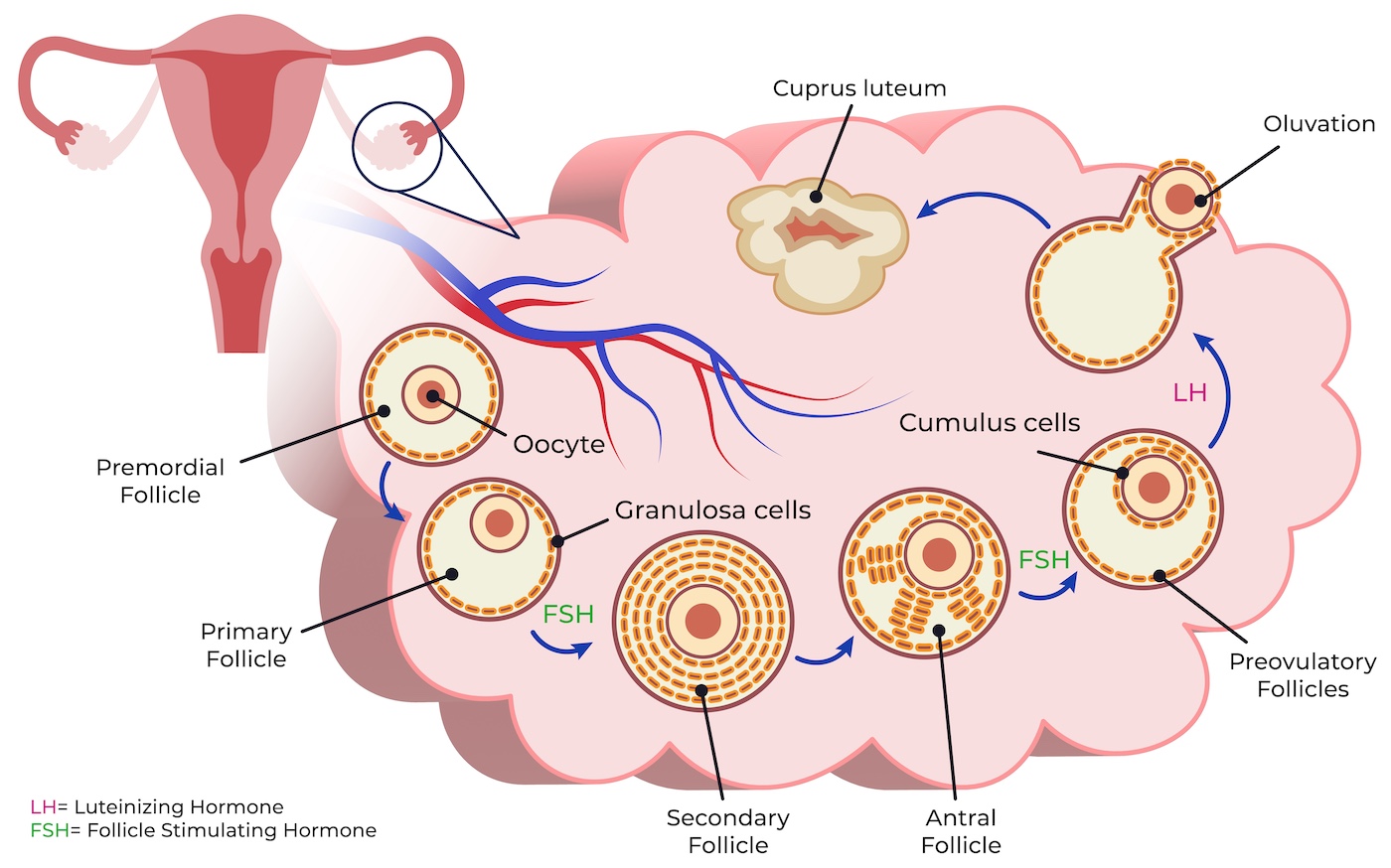
Adapted from: Shareghi-oskoue, O., Aghebati-Maleki, L. & Yousefi, M. Transplantation of human umbilical cord mesenchymal stem cells to treat premature ovarian failure. Stem Cell Res Ther 12, 454 (2021). https://doi.org/10.1186/
How does FSH impact fertility?
Follicle stimulating hormone is the hormone that recruits a group of follicles (premature eggs) each cycle and jump-starts their growth—one of which will become the dominant follicle and the chosen egg to be ovulated that cycle.
After the group of follicles are recruited, FSH turns on an enzyme called aromatase that will take androgens in those follicle cells and turn them into estrogen. This is an important step in egg development since estrogen helps continue egg development and triggers ovulation. The more the egg grows, the higher the estrogen. When the egg is fully developed, those high estrogen levels will cause a surge in Luteinizing Hormone (LH) which triggers ovulation—the release of the egg.
This process of egg growth and ovulation that is supposed to occur each reproductive cycle can get derailed if the FSH signals don’t get through properly. This can happen in PCOS and other cases of infertility or subfertility. When follicle growth is delayed or halted it can cause long cycles or may stop ovulation from occurring altogether.
How does insulin affect fertility and PCOS?
Insulin is most well known as the hormone that controls blood sugar levels, but when unregulated, it can also interfere with ovarian function. That’s because the ovarian follicle cells have insulin receptors.
When the body is continuously exposed to elevated insulin, our cells can become less sensitive to it—also called insulin resistance—resulting in higher insulin levels in circulation (even when you’ve been fasting overnight for 8 to 12 hours). Insulin resistance and abnormally high insulin levels are strongly associated with PCOS and its progression, regardless of BMI. One study reported that 62% to 95% of females with PCOS had insulin resistance, and this included females with lean body compositions as well as those who were overweight or obese.3
Continuously having high insulin in circulation is a problem because all of that insulin can travel to the ovaries, attach to the follicle cells and cause 1) increased sensitivity to LH, and 2) increased androgen production. Being too sensitive to LH means that ovulation could be improperly timed (too early, too late, or not at all). Meanwhile, excessive amounts of androgens can interfere with follicle development. So having poor insulin regulation can actually impede both egg development and ovulation.
How does Myo-Inositol improve fertility in PCOS?
Inositol is an insulin sensitizer. When insulin attaches to its receptors, it starts a cascade of signals that brings glucose transporters to the cell membrane, like a tunnel that allows glucose sugar to enter. Inositol enhances these signals, activating glucose transporters so that sugar can move from the bloodstream into your cells. This decreases the amount of actual insulin your body needs to release, lowering the amount of circulating insulin.4
In general, any treatment that reduces high insulin levels will improve androgen levels and ovulation in PCOS. Myo-Inositol is the messenger that does this by improving both insulin sensitivity and FSH signaling.
In a 2009 study, 42 females with PCOS (having long or irregular cycles and high testosterone) were given either 400mcg folic acid or the same amount of folic acid with 4g MI daily for six weeks. At the end of the study, those given MI had significant reductions in free and total testosterone and improvements in insulin sensitivity.5 Fertility-wise, about 70% of those with PCOS given MI ovulated compared to 21% in the control group.

Can Myo-Inositol be used in IVF cycles?
Since MI can improve FSH sensitivity, it can be used to improve the response to recombinant FSH (r-FSH) medications in treated cycles like intrauterine insemination (IUI) and in-vitro fertilization (IVF) while reducing the required dose.
In a meta-analysis that included 935 females with PCOS, the daily use of MI before an IVF cycle led to significantly greater clinical pregnancy rates (33.3% in the MI group versus 27.6% in the control group).6 Additionally, in the three studies that reported miscarriage rates, groups given MI had significantly lower rates of pregnancy loss (5.9% versus 27.6% in control groups).
Does Myo-Inositol affect embryo quality?
The presence of a high ratio MI to DCI in the follicular fluid has been associated with better embryo quality compared to high amounts of DCI and low MI.2 In particular, MI’s role in cell signaling activates the cell cycle that results in the development of the embryo. With its antioxidant properties, MI can also help reduce oxidative stress and damage.
In a study of females with PCOS who were under the age of 40 years, taking 4g MI and 400mcg folic acid for three months before undergoing IVF with ICSI (intracytoplasmic sperm injection) resulted in significantly reduced doses of r-FSH compared to those given folic acid only.7 The MI group also had significantly more mature oocytes retrieved, significantly less degenerated eggs, and a greater number of grade 1 embryos (those with cells of equal size and no fragmentation).
In summary, myo-inositol enhances the signaling of key hormones FSH and insulin—both of which affect fertility. Myo-inositol has been shown to promote ovarian follicle recruitment, development and support egg quality. Meanwhile its effects on insulin signaling help reduce hyperinsulinemia and diminish the interference that excessive insulin can have on ovarian function. These properties support the use of MI in females with PCOS.
Summary of effects of MI:
- Decreases insulin levels and insulin resistance
- Decreases excess androgens
- Improves FSH function
- Promotes the proper timing of ovulation
References
- Nordio M, Basciani S, Camajani E. The 40:1 myo-inositol/D-chiro-inositol plasma ratio is able to restore ovulation in PCOS patients: comparison with other ratios. Eur Rev Med Pharmacol Sci. 2019 Jun;23(12):5512-5521. https://pubmed.ncbi.nlm.nih.gov/31298405/
- Chiu TT, Rogers MS, Law EL, et al. Follicular fluid and serum concentrations of myo-inositol in patients undergoing IVF: relationship with oocyte quality. Hum Reprod. 2002 Jun;17(6):1591-6. https://pubmed.ncbi.nlm.nih.gov/12042283/
- Stepto NK, Cassar S, Joham AE, et al. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013 Mar;28(3):777-84. https://pubmed.ncbi.nlm.nih.gov/23315061/
- Gambioli R, Forte G, Buzzaccarini G, et al. Myo-Inositol as a Key Supporter of Fertility and Physiological Gestation. Pharmaceuticals (Basel). 2021 May 25;14(6):504. https://pubmed.ncbi.nlm.nih.gov/34070701/
- Costantino D, Minozzi G, Minozzi E, Guaraldi C. Metabolic and hormonal effects of myo-inositol in women with polycystic ovary syndrome: a double-blind trial. Eur Rev Med Pharmacol Sci. 2009 Mar-Apr;13(2):105-10. https://pubmed.ncbi.nlm.nih.gov/19499845/
- Zheng X, Lin D, Zhang Y, et al. Inositol supplement improves clinical pregnancy rate in infertile women undergoing ovulation induction for ICSI or IVF-ET. Medicine (Baltimore). 2017 Dec;96(49):e8842. https://pubmed.ncbi.nlm.nih.gov/29245250/
- Ciotta L, Stracquadanio M, Pagano I, et al. Effects of myo-inositol supplementation on oocyte’s quality in PCOS patients: a double blind trial. Eur Rev Med Pharmacol Sci. 2011 May;15(5):509-14. https://pubmed.ncbi.nlm.nih.gov/21744744/
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third-party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/